Low uptake of contraceptives in rural areas worrying

Locadia Mavhudzi Features Correspondent
While women in urban areas are exposed to a variety of family planning choices, the plight of women in rural and peripheral areas with regards to access to contraception is still miserable. A recent visit to Mambowa small scale mining area in Shurugwi revealed that many young women who entered into marriage at an early age did not have access to contraceptives and in the case that family planning choices are available, they cannot afford the costs.
Muchaneta Machirori, a 22- year-old mother, with three children below five years, said she has never used any contraceptives for a long time due to various reasons.
“We normally get lessons on the need to use contraceptives when we visit the clinic for baby wellness but I cannot afford the one dollar cost that is needed for pills,” she said. Way back in the village, Machirori said, health workers used to distribute family planning pills for free but it is now a thing of the past.
“Our village health workers used to supply us with family planning pills but now they no longer do so. I wish that system would be brought back because it empowers me as a woman to control my reproductive system,” she said. Machirori said her three children who are aged five, three and one are not by choice.
“My biggest fear is that I might even fall pregnant again because once I stop breastfeeding I will be susceptible to another pregnancy,” she said. The mother of three revealed that she had in the past tried traditional forms of family planning but the methods came in with their own side effects.
“Our village traditional midwives have told us about some traditional herbs such as “mutsvanzva, munhanzva and roots of a ‘‘muroro” tree but these have not been very efficient. The labour of having to go into the forest every now and again and at times overdose of the prescription may lead to further health complications”, she said. The young woman, said the burden of family planning rests upon her as a woman because her husband is not interested in the subject.
“I always tell my husband to buy me family planning pills but he does not take it as a serious issue,” she said.
“When I fall pregnant, it becomes my burden to cater for the child until the child goes to school. My husband does not share the challenges I go through in raising the children. He only shows joy when a baby boy is born.” Family planning the world over has long been fraught with political, cultural and religious controversy, ever since the first pioneers began to promote the benefits of birth spacing in the early 20th century.
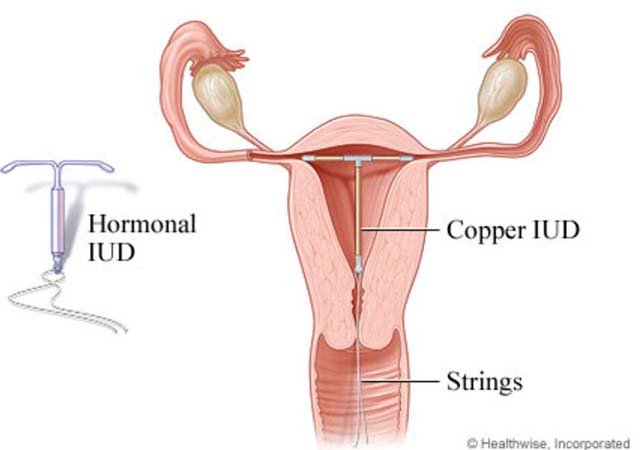
According to statistics released by the Zimbabwe National Family Planning Council, the uptake of family planning is still low in rural areas where teenage pregnancies are still prevalent. Knowledge of contraception means knowing at least one of the methods of family planning. Modern contraceptive methods include female sterilisation, male sterilisation, the pill, the intrauterine device (IUD), injectables, implants, male condoms, female condoms, the diaphragm, foam/jelly, the lactational amenorrhea method, and traditional methods include periodic abstinence and withdrawal. Women rights activist Nyaradzo Mashayamombe believes women’s empowerment should go beyond the boardroom talk.
“Provision of family planning services in rural areas should be free and accessible,” she says.
“That alone will prevent a lot of child marriages that are rampant in rural settings. If male condoms are readily available in many places, then why not family planning services and sanitary pads for women? “
Meanwhile, lawmakers recently called on government to channel more funds towards family planning and reproductive health as they are currently largely dependent on donor funds. Chairperson of the Parliamentary Portfolio Committee on health, Dr Ruth Labode, noted that there is an urgent need to mobilize funds for family planning services especially in rural areas.
Population Services Zimbabwe country director, Abebe Shibru said family planning has advantages in that it improves the health, education, and well-being of women, as well as allowing countries to invest in economic development. No operations and capital grant was availed to the Zimbabwe National Family Planning Council by the government from 2014. Dr Munyaradzi Murwira, director of the Zimbabwe National Family Planning Council, noted the challenges associated with boosting contraceptive use in the country.
“The problems about funding gaps is nothing new, as funding for family planning was diverted to HIV programmes across the developing world during the 1990s,” he said.
“Funding for our family planning programmes has been limited over the last 10 to 15 years. Barriers to meeting the full demand for contraceptives are many. Stock outs limit access to contraception, some countries limit contraceptives on non-medical grounds, for example, to unmarried women and adolescents, and some women need their husbands’ consent to use contraception or must pay for it.”
The unmet need for contraceptives among married women aged 15-49 years in WHO’s Africa Region is estimated at 24 percent and lags considerably behind the rest of the world, according to the Atlas of African health statistics 2016. However, Zimbabwe remains one of the top countries to scale up health services in Africa. Critics believe high literacy rates in Zimbabwe, should reflect a knowledgeable and progressive society that is able to make healthy choices.
According to the 2015 Zimbabwe Demographic Health Survey – the country exceeds the global average on contraceptive prevalence in sub Saharan Africa with 67 percent of married women aged 15 to 49 years having access to contraceptives. Zimbabwe’s family planning strategy is to increase contraceptive prevalence rate from 59 percent to 68 percent by 2020, and in the process reducing teenage pregnancies from 24 percent to 12 percent by 2020.










Comments