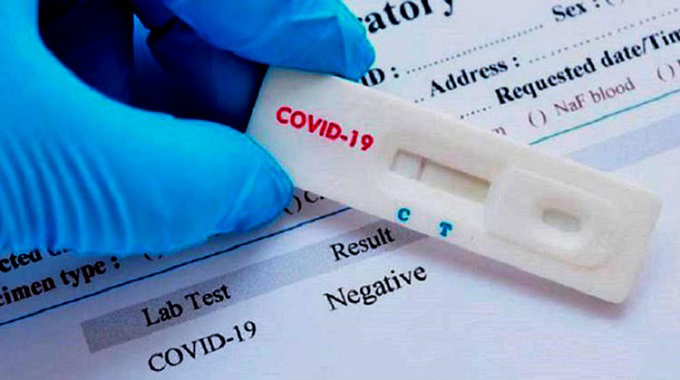
Third wave of Covid-19 put a strain on maternal health services
Rumbidzayi Zinyuke
Health Reporter
The third wave of Covid-19 infections currently being experienced have put a strain on maternal health services in rural Zimbabwe, where pregnant women in remote areas are failing to access timely care.
Since the beginning of Covid 19 last year, women in most African countries, Zimbabwe included, could not easily access health centres due to lockdowns that restricted movement.
Although the situation had become better with the easing of the Covid-19 restrictions, the recent surge in cases meant new lockdown measures and the return of the problem for some areas.
Although health services have continued to be provided at all institutions, for villagers in Rural Buhera, accessing the hospitals has been a challenge due to transport challenges.
Although authorities in the district do not have a figure of how many women have been affected, Buhera District Medical Officer Dr Shelton Kwiri said there had been an increase in the number of home deliveries being recorded.
“During this current wave, we have tried to maintain all other services at our hospitals and clinics running to ensure that we provide healthcare to all patients. We have a huge number of patients on ARVs and other chronic disease treatment and they want services so we are trying to make sure there is continuity.
“However, we have noticed an increase in community deliveries. We are yet to do a proper assessment to discover the reason behind this,” he said.
Dr Kwiri said the district would conduct a situation analysis of the effect that covid-19 has had on maternal health service delivery.
The most likely reason for the increase in the number of home deliveries could be the shortage of transport.
“Buhera has no tarred road and during this lockdown period, there has been a shortage of reliable transport. Because of a poor road network, there are no buses to provide alternative transport so people have to rely on mushikashika to get to the hospital and these are expensive,” said Dr Kwiri.
For a journey of 50km, villagers are having to fork out at least US$7, which is expensive for the women, most of whom have to be accompanied by a relative to the hospital.
Those who fail to travel the money then opt for home deliveries or wait until it is too late to travel to the hospital.
As a result, fewer women then get to have proper care at a health facility and this could potentially lead to an increase in maternal mortality rates.
According to the United Nations Population Fund (UNFPA), as of 2019, Zimbabwe had a high maternal mortality rate of 462 deaths per 100 000 live births.
“Our communities are not giving us all the information so we might be having a high number of women in this situation. We want to see how we can improve on our surveillance system on maternal and neo natal deaths. Since we now have more community deliveries, we are also likely to be having some deaths but this has not yet been factored into our reporting,” Dr Kwiri said.
During the peak of the first wave of Covid-19 infections, the World health Organisation in Africa warned of a rise in maternal deaths in several countries as curfews imposed by Governments made it difficult for pregnant women to reach the health facilities on time.
Recently, deputy director HIV/STIs programme in the Ministry of Health and Child Care Dr Tsitsi Apollo told delegates at the Uniformed Forces Health Service conference that some health facilities had decongested waiting mothers’ shelters due to the Covid 19 pandemic hence institutions had recorded late bookings for antenatal care from the women, most of whom stay far from the hospitals.
She said there was need for clear guidance on maternal health issues in the context of Covid 19.









Comments