If you are infected: demystifying Covid-19 care

Dr Satchit Balsari, Dr Zarir Udwadia
After three months of missteps, there seems to be consensus — or rather a late realisation — that not all patients with Covid-19 need to be taken to hospitals. We have known with fair certainty since early March that Covid-19 does not spread like Ebola, and that in the absence of effective medical treatment, non-pharmaceutical interventions like hand-washing, masking and physical distancing would be the best defence.
And yet, for nearly one hundred days, confirmed cases of Covid-19 in India’s cities were being admitted to hospitals, irrespective of the severity of disease.
This blunder — with no clinical justification — resulted in first paralysing, then overwhelming, and finally crushing entire health systems. The hospitals were rendered incapable of caring for tens of thousands of other patients with non-Covid-related diseases, and jeopardised the wellbeing of their overworked staff. What can other cities, towns and villages in India learn from this, as the pandemic spreads to the hinterland?
Explained | The G4 flu virus with ‘pandemic potential’, found by Chinese researchers?
There are a finite number of permutations that can occur, when someone is exposed to Covid-19. Let’s walk through these possibilities, and the possible care pathways each situation warrants.
Asymptomatics: If exposed, one gets Covid-19 or one doesn’t. Of all who get it, most will be asymptomatic: they will show no symptoms, but will continue to spread it. It is likely that they may be less contagious than someone who is actively coughing, but there is no evidence to suggest that the asymptomatic patients do not spread the virus. They, however, need no treatment.
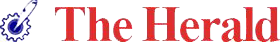
Presymptomatics and mild cases: Of the few that are symptomatic, all will first be pre-symptomatic. This is the roughly two-day interval in which they will be contagious, will spread the virus, but will not have developed symptoms. Eventually they will develop one or a combination of the Covid-19 symptoms we recognise: loss of smell or taste, cough, fever, and so on.
Most of these symptomatic cases will only have mild symptoms and will also need no treatment, except what physicians appropriately call “symptomatic management”, with medications to simply manage the fever and cough and bodyaches. Home remedies may help with some of this, but there is no evidence that they alter the course of the disease.
Symptomatics, moderate: Of the remainder, some will develop moderate symptoms, and some will develop severe disease. Only these two categories need sophisticated medical intervention.
Explained | What is Covaxin, India’s Covid-19 vaccine candidate?
coronavirus, coronavirus news, india coronavirus, coronavirus news, coronavirus india, coronavirus cases in india, india coronavirus cases, coronavirus latest news, coronavirus update, india coronavirus update, covid 19, covid 19 india, india covid 19, covid 19 tracker, india covid 19 tracker, corona cases, corona news, corona cases in india, total corona cases in india Municipal authorities in Mumbai with the help of local politicians and corporators hold fever and testing camps at various coronavirus hotspots.
Those with moderate symptoms will benefit from oxygen therapy, and “pronation,” which in plain English, means lying on your belly, instead of your back. Doing so opens up the air chambers in the back of your lungs that are normally collapsed, thereby providing more oxygen to your blood. Early evidence shows that this helps avert the need for more aggressive intervention in some cases.
But the principal intervention for those with moderate severity is oxygen — which can be delivered through a mask and tube connected to a portable oxygen tank (which like a gas cylinder, is heavy, and must be replaced); or as piped oxygen, as is available in some hospitals, and which comes from larger tanks; or simply via a small, portable machine called an oxygen concentrator which makes oxygen from air. Many people with lung diseases have them at home. There is no clinical justification to take up ICU beds for these patients. They do not need ventilators, or intensive care specialists — especially when no city in India has enough of either, and most smaller towns and villages have neither.
Severe cases: Unlike run-of-the-mill pneumonias, we have observed that the shortness of breath in patients with Covid-19 can progress abruptly, and these patients need ventilators. These breathing machines are highly complex systems that need skilled technicians to run them, and require that patients have a flexible plastic tube advanced into their trachea (windpipe), typically by an anaesthesiologist or emergency physicians or intensivists. The patients then have to be kept sedated (asleep) with a precisely dosed intravenous medication — an overdose of which can easily kill the patient. And finally, plasma donated from Covid-19 survivors helps some of the sickest. These are the critical elements of an “ICU bed” — there is nothing special about the bed itself.
Express Explained is now on Telegram. Click here to join our channel (@ieexplained) and stay updated with the latest
coronavirus, west bengal covid deaths, Kolkata covid dead body kept in home, west bengal covid funerals, bengal covid funeral rules, west bengal covid cases, coronavirus cases Most of these symptomatic cases will only have mild symptoms and will also need no treatment
Community-based care: The best way to relax the load on hospitals is to keep all those who do not need hospital-based care, away from hospitals — for as long as is safely possible. Keeping people home safely means monitoring symptomatic patients by measuring their respiratory rate (counting how many breaths they take per minute — the average person takes about 12) and their oxygen saturation, using a small device that clips on to your fingertips, called pulse-oximeter. Neighbourhood champions and community health workers can be easily taught to do this via online teaching aids.
If the oxygen saturation begins to go down, or the respiratory rate begins to go up, the patients need intervention — first, oxygen therapy. Most will not have access to hospitals, and can be safely given oxygen at home when possible, or in neighbourhood Covid-care centres. A minority will have to go to hospital.
There will, of course, be many exceptions to this neat linear progression, but the vast majority will follow this trajectory, as data from around the world are showing. (We still don’t have reliable clinical data from India.)
This strategy is not new. By early April, patients in New York, where the epidemic was then at its peak, were being sent home with pulse-oximeters and even oxygen concentrators. Various states in India were at the time embracing unproven, unvalidated interventions.
Instead of distributing spice mixtures, arsenicum album and hydroxychloroquine, it will now be wiser to distribute pulse-oximeters to communities at risk. So far, early data suggest that a steroid and the antiviral remdesivir may show some benefit in more severe hospitalised cases. Favipiravir has been approved for use in moderate cases in India, but the data have not been released. Note however, that a similar wonder-drug for influenza mostly brings down symptoms by a day. These medications are not cures.
Covid-19 will ravage neighbourhoods across India. The best strategy will be to mount a hyper-local response that is backed by science. Dharavi and Kerala — very different from each other — have shown how a highly context-driven strategy works. Most of those who will get Covid-19 will be fine. Among those who have some symptoms, monitor as many as possible with pulse-oximeters (or simply by counting the respiratory rate, when devices run out). And if short of breath, administer oxygenation and pronation.
A minority will get very sick, and will require critical care. The harsh reality is that most from the last group will not get the care they need. We cannot fix decades of neglect while in the throes of a pandemic.- The Indian Express
- (Dr Satchit Balsari is assistant professor in Emergency Medicine and in Global Health at Harvard University’s medical and public health schools. Dr Zarir Udwadia is Consultant Chest Physician, PD Hinduja Hospital & Medical Research Centre, Mumbai)





Comments