Global experts speak on vaccines misconception
Roselyne Sachiti
Features, Health & Society Editor
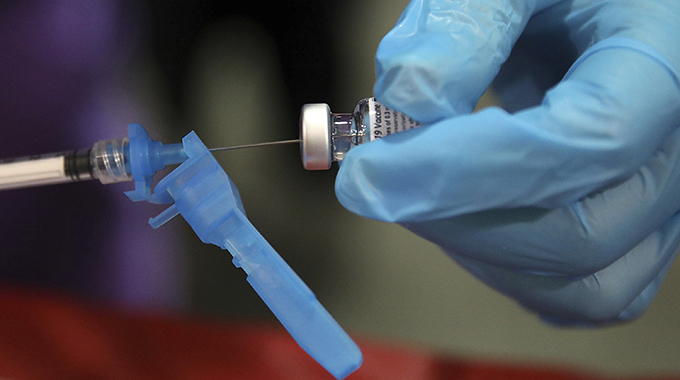
Zimbabwe is expected to receive its first batch of Covid-19 vaccine next month, with the Government now finalising its national deployment plan and training of health care workers who will administer the inoculation.
The country is preparing to take delivery of the vaccine procured under a global ground breaking initiative led by the World Health Organisation, known as Covax, which plans to procure and distribute a billion doses to African countries once licensed and approved.
The initiative will see two billion doses distributed equitably in all participating nations.
As the country is readying itself to take delivery of the vaccines, misinformation on social media platforms on the danger that vaccines pose, myths and misconceptions and mistrust have been doing rounds, creating uncertainty among the people.
Citing some conspiracy theories, some people are circulating information on how the Covid-19 vaccines will have long-term side effects, and that those who take them will ultimately die. Some say the vaccines affect fertility, and the list is too long, depressing and exhausting, but all without any scientific proof.
Some religious leaders in Zimbabwe have also become the biblical doubting Thomases, encouraging their followers not to take the vaccines.
What do scientists from around the globe say about the efficacy of vaccines?
Speaking during a HIV Research for Prevention (HIVR4P) Virtual Journalist Fellows Session titled: “Covid vaccines and treatments” last week, professor of Clinical Investigation and senior attending physician at The Rockefeller University, New York, US, Sara Schlesinger, explained that Covid-19 being a brand new virus, the most experienced people in the world have only known its sequence for one year.
“In that time, all of our lives have been changed,” she said. “The pandemic has swept through the world like nothing we have ever seen, and the responses have been the same.”
According to Prof Schlesinger, the most remarkable thing is that in less than a year, there is a 95 percent efficacious vaccine.
“That in my mind is nothing short of a full blown miracle,” she said. “Everyone is reluctant to speak so enthusiastically about that miracle for fear of people letting their guard down.”
Prof Schlesinger said so much like HIV, there were other kinds of prevention activities that people had been doing and continued to do.
These include wearing face masks, social distancing, staying at home and washing of hands. She said while none of these were interesting to talk about, none are scientifically novel, but they all work.
“You have a sort of dichotomy of this brand new catastrophe virus that can be fought with measures my grandparents, who were physicians and graduated in the 20s, advocated,” said Prof Schlesinger.
“Yet we have managed through our biomedical research community to develop and deploy a vaccine, more than one vaccine, many vaccines.”
Prof Schlesinger said there has been huge progress in identifying the virus, sequencing it, making the vaccine to combat the virus, and while doing that figuring out what works medically both in terms of treatments and less technical kinds of prevention.
“Like wheels, all of these pieces are moving together, but when time comes in, the virus starts to change,” she said.
She said one of the topical things to be discussed at the ongoing HIV Research for Prevention (HIVR4P) Virtual Conference was how the virus was changing across the globe and what that meant for the vaccines and the path of the pandemic and for treatment.
“While these trials were put together rapidly, they have been executed, in my view, brilliantly,” said Prof Schlesinger. “What we know is these vaccines are very safe. I keep getting questions from colleagues, friends, people at work. The question is ‘are they safe since they have been developed so quickly?’ From what we know we have been very fortunate that these vaccines are very safe.”
Prof Schlesinger said another question people usually ask is “do the vaccines work and what do they prevent?”
“No vaccine that I know of completely shuts down a virus when you encounter it after the vaccine,” she said. “That is a challenge with an HIV vaccine because of things that are special about HIV.”
Added Prof Schlesinger: “Fortunately, Covid-19 is more like the traditional viruses for which we are protected with vaccines among them measles rubella. So, if you encounter a small amount of virus after you have been vaccinated, your body wakes up and remembers the key things about immune responses and makes an immune response and protects you.”
From an individual point of view, said Prof Schlesinger, who also received a Covid-19 vaccine, “the vaccines are terrific, are safe and work to protect from severe disease and actually from infection so they keep people safe.”
She said none of the vaccines that were being deployed will have the possibility of giving people Covid-19.
“But, it is completely possible to get Covid-19 after you have been vaccinated, before you fully make an immune response,” she said. “That concept that it takes two weeks after the second shot. If you get your first shot and its four weeks later and its two weeks after that (and that’s six weeks after your first shot) that you are still vulnerable. The vulnerability goes down and if you look at the curves it goes after 12 days. Understanding those kinetics is very important. It does not mean the vaccine caused the infection, it means the person remained vulnerable,” she said.
Prof Schlesinger added that it is also important to discuss risk.
“No one would take a vaccine that has been developed under these circumstances if we were not in a pandemic,” she said. “We would wait for more safety data, but we are in a pandemic. One has to think very hard about what the risks are for the individual from the vaccine and from acquiring Covid-19. What are the risks from the vaccine and what are the risks from acquiring Covid-19?”
Executive director of the Wits Reproductive Health and HIV Institute, University of Witwatersrand and professor in the Department of Obstetrics and Gynaecology, Helen Rees, said the vaccine trials typically have a common endpoint, PCR, a laboratory confirmed infection.
“Then there are a lot of secondary endpoints that people are looking for. There are some slight differences there, but what would be to say the severity of the infection, the time between vaccination and when the infection arises. Clearly safety is part of that primary evaluation as well,” she said.
According to Prof Rees, some of the vaccines are also trying to see what happens in terms of asymptomatic infection.
“That’s by swabbing people in the trial on a weekly basis, we to try to see if there is an asymptomatic infection that can be detected,” she said. “To summarise from what we know from most of these big clinical trials at the moment is that we know about safety, often in tens of thousands of people anything from 20 000 or 30 000 and then going up.
“We now know about safety of that number of people for a short period of time often about two months in the first instance and then followed up for longer.”
Prof Rees said they now know a level of efficacy; how good a vaccine is in preventing a laboratory confirmed infection.
“We measure how good is it,” she said. “Is it 70 percent for the Astra Zeneca one or is it 95 percent for the Mordena or a little bit less for Pfizer. We know how effective it is.
“What we do not know at the moment, for any of the vaccines, and this is work that still has to be done and important if we want to break community transmission of the virus, is: does it have an impact on transmission of the virus? That is something that we still have to understand. If what it does is lowering the severity of the infections, which is excellent, but we are still getting transmission of the virus despite being vaccinated, that will mean we will be less likely to interrupt transmission at a community level.”
Professor of Mucosal Infection and Immunity at Imperial College, London Robin Shattock said common to all the trials is protection from disease rather than PCR detection without disease.
“Some of the trials have looked at PCR only even if they are asymptomatic, but the majority have not,” he noted. “Right now we have no information on their ability to prevent transmission. Everyone assumes they will have some ability to prevent transmission.
“It is important to differentiate the impact on transient infection of an individual versus the impact on transmission at a population level.” Prof Shattock explained that what makes that very complex is in many countries a number of vaccines are being rolled out at the same time.
“Some vaccines may be better than others at reducing transmission rates,” he said. “To get a real handle on that we may have to be looking at countries that are exclusively using only one of the vaccines that are currently being approved otherwise it may be difficult to untangle the data. We need more vaccine doses and whether that’s through increasing capacity of those that have proved to work or whether bringing other vaccines that have manufactured using different supply chains.”
Director of United States-based National Programs for the Black AIDS Institute, Rob Newells, said in the US, politics has played a huge role in how Covid-19 is seen by the public. He said engaging the community around Covid-19 research has been different than HIV research. People, he said, were paying attention to Covid-19.
Feedback : [email protected] or [email protected],or Twitter @RoselyneSachiti










Comments