Covid-19 could be catalyst for top-notch health delivery system
Lovemore Chikova Development Dialogue
Achieving a top-notch health delivery system in light of Covid-19 might be a huge task for countries like Zimbabwe, but with partnerships between the public and private sectors, improvements can be registered.
The outbreak of Covid-19 has shown how such partnerships can work for the good of the country in terms of perfecting the health system.
The private operators who have been giving a hand in the fight against the spread of Covid-19 by donating various items to the health sector should be encouraged even after the fight against this disease is over.
This comes in the wake of Government announcing the intention to establish at least 67 heath centres across the country to cater for Covid-19 cases. These health centres should not be concentrated in urban areas alone, but should be spread to rural areas where the health system is lagging. Such health facilities will continue to be used by the local communities when their use for Covid-19 issues is no longer necessary.
In recent days, Sakunda Holding committed US$2,7 million towards the refurbishment of Rock Foundation Medical Centre and St Anne’s Hospital in Harare. These two hospitals were not functioning for different reasons, and their revival will not only contribute to the fight against Covid-19, but to the resurgence of the health system.
To aid its work, Sakunda Holdings said it was bringing into the country 100 ventilators, 10 000 rapid test kits, 10 000 disposal protective gowns, 20 000 medical masks, 10 000 disposable shoe covers, 100 infra-red thermometers, 5 000 respirator N95 masks and 2 000 hand sanitisers, among other paraphernalia required to fight Covid-19.
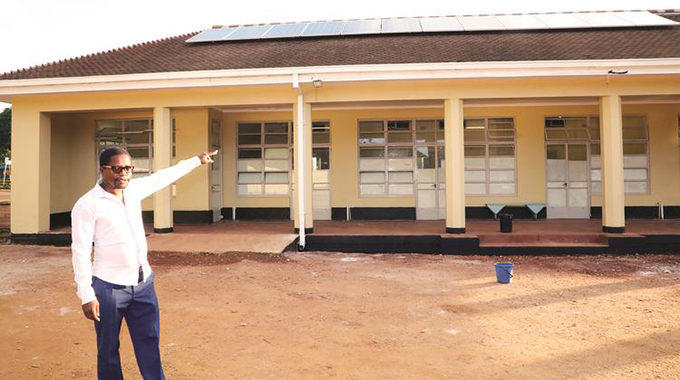
More partners have been coming in to help transform institutions such as Ekusileni Medical Centre in Bulawayo and a hotel in Beitbridge into top-notch health centres that can also deal with Covid-19.
Government partnered the Chinese business community and local businesses in renovating Wilkins Infectious Diseases Hospital in Harare to make it the major referral centre for Covid-19 patients. This hospital, together with Beatrice Road Infectious Diseases Hospital, also in Harare, will continue serving the city after Covid-19, with many residents benefiting from such a partnership.
Some private hospitals have been at the forefront of instituting measures that help with the detection of suspected Covid-19 cases at their institutions. One such hospital that has set up an elaborate system that feeds into the broader efforts to term the spread of Covid-19 is Health Point. At this hospital, visitors arrive at a screening pod where they wash their hands, put on a mask and have their temperature recorded.
Anyone who turns out to be feverish is taken to a second pod for assessment and isolation where a casualty officer tries to establish the causes of the elevated temperature.
If there are reasonable suspicions of Covid-19, the hospital then works with the broader Covid-19 system to ensure the patient is further managed in that regard.
What the private partners have done so far is an indication that with proper interventions, Zimbabwe’s health sector can be transformed and get to the levels everyone desires. If external resources are directed to the health sector, it means less burden on the fiscus, which is already burdened, especially in light of Covid-19.
The importance of partnerships in the health sector is that they help mobilise a diverse range of stakeholders and focus attention on specific issues with a potential to transform the sector.
It is then crucial that Government extends the concept to a variety of stakeholders even after Covid-19 so that synergies are formed to mobilise the much needed resources in enhancing the health sector.
Partnerships have proved useful in strengthening health systems, including maternal and child health programmes, the prevention and control of communicable and non-communicable diseases, and in tackling the key determinants of health.
In its quest to have these partnerships, the Government should not neglect the rural areas where the health delivery system is already affected by different aspects that hinder its efficiency. Access to health services has since become an integral part of rural development, calling for more resources to be directed towards the rural areas.
In case of Covid-19 cases being detected in marginalised areas, there is likely to be difficulties in managing them considering the long distances travelled to health service centres.
It is then clear that a vibrant rural health system is necessary, and through partnerships, Government can easily build a resilient system, not only for Covid-19, but for other health needs.
Although there have been improvements in health access in rural areas in Zimbabwe in recent years mainly due to the spread of technology, many such places still remain margnalised.
Advances in medical research and public health are yet to fully benefit people in the rural areas, yet most of the people in the country live in such areas.
There are both human and geographical determinants of access to health that need to be dealt with, not only by Government, but other partners, especially those from the private sector.
And there are various strategies and policies that can be considered to upscale access to health in rural communities in the light of Covid-19, but these need to be tackled holistically.
The purpose should be to close the great divide between access to health and the quality of health services in rural areas and urban areas.
The partnerships discussed above are in most cases directed to the urban areas at the expense of rural areas, further marginalising the rural communities on access to better health services.
The advent of Covid-19 should result in private partners availing equipment like mobile clinics to the rural areas and ensure the service continues to exist even after the coronavirus is defeated.
Mobile clinics can help scale up access to primary health care quickly and effectively because they are cheaper to operate and come with less costs to rural communities.
Partnerships in the health sector can actually result in the private sector sponsoring qualified health workers to be deployed in rural areas, which they shun because of poor working conditions. Incentives can be offered to such critical health workers. Such partnerships can also result in rural health centres being equipped with necessities such as electricity, running water and other equipment.
Primary health care givers, mainly community health workers can also be empowered through partnerships to enhance access to health in rural areas. The community health workers can easily help people identify causes of health problems which the authorities can address to prevent outbreak of diseases.
In such times of Covid-19, health development partners can help marginalised areas with availing information communication technologies like mobile phones, which can be used to disseminate information about health from experts.
Through such mobile phones, rural people can get information on how to avoid catching Covid-19 and stay healthy.
In considering partnerships in the health sector, it then imperative that the partners and Government consider upscaling health access in rural areas which are usually the most affected, yet the people there have low capacity to cope.






Comments