A step towards HIV Cure . . . as WHO works on gene therapy guidelines

Catherine Murombedzi
Correspondent
WITH the human immuno deficiency virus (HIV) mutations standing over a million, the HIV cure and vaccination research is all hands on the deck, with various clinical trials taking place.
Each clinical trial informs on the next step, with lessons learned of what can be done.
The World Health Organisation (WHO), in December 2021 released draft gene therapy guidelines and is compiling feedback from stakeholders to issue the final document.
The guidelines will open up for ministries of health to formulate in-country plans, processes and strategies for gene therapy at national level.
An informative virtual science cafe on HIV cure research was recently held, with the Health Communicators Forum (HCF) of Zimbabwe sensitised by a Ugandan researcher, Dr Cissy Kityo in the interactive discussion.
The HCF is hosted by the Humanitarian Information Facilitation Centre, (HIFC) with science cafes supported by Avac.
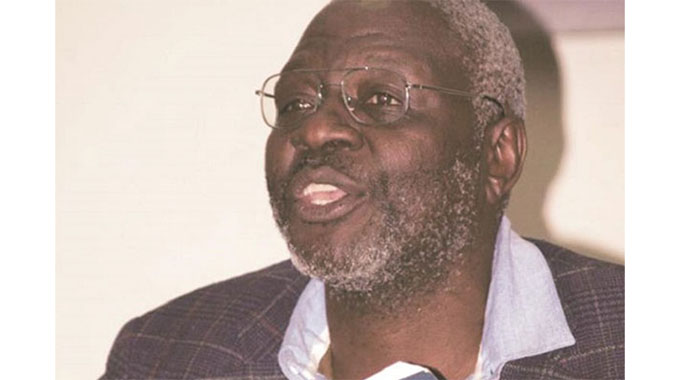
Dr Kityo, a Ugandan researcher has been in the HIV field since 1990 when clinical trials for treatment took place.
She has participated in treatment outcomes and remains committed to being part of the HIV Cure journey.
While many dismiss an HIV Cure as far-fetched, to science, everyday is a learning curve, an inch towards HIV Cure is.
Dr Kityo simplified science for the HCF to enable health science journalists to be able to disseminate information correctly.
She gave an example of a house under construction which requires a plan.
The building follows the laid out plan. So do our bodies, everyone has a DNA, which is what makes the functions of the body.
Our bodies follow a sequence too, a genetic order.
As a researcher undertaking gene therapy, she talked of the two main therapies under their research project.
“The two types of gene therapy under trial are ex-vivo and in-vivo,” said Dr Kityo. “In the ex-vivo gene therapy, target cells are removed from the patient’s body, genetically modified and put back into the patient’s body.
“The corrected cells are then re-infused into the patient,” explained Dr Kityo, in the interactive virtual meeting. The other intervention is the in-vivo, which has successfully been used in the treatment of blood diseases, specifically blood cancer.”
Dr Kityo said the in-vivo procedure takes place inside the patient’s body.
“This is done inside the patient’s body through an injection which will genetically modify the cells,’ she said. “The target cell may be T cells which then grows resistant to HIV. The cell grows extensions, thereby replicating to replace the damaged cells.
“The patient is monitored and with this success, gene therapy is set to be the front runner as it will require no donor. The patient’s genes are the ones genetically modified.”
Donor Cells
To date, only five cancer patients have been cured of HIV using stem cell transplant.
The stem cells were all donated. Finding matching donors also takes time and the procedure is very expensive, requiring state-of-the-art hospital settings and expertise.
With an estimated 38+ million people living with HIV globally, it is impossible to find matching donors.
So gene therapy mimics what happened to the five patients and requires no donor as the patient’s cells are the ones which go under modification.
A similar method in cancer treatment, where a patient is given chemotherapy is used in stem cell, which takes root in virgin bone marrow.
The cells start to mutate similar cells which are HIV resistant.
The beauty of HIV gene therapy is that no donor will be required, Dr Kityo educated the forum.
Clinical Trials
In the 1990, ARVs were on clinical trials, the reality was a mirage. Research did not hesitate, patients took the trials, today, drugs keep improving with better outcomes.
Someone took the trials for HIV treatment, someone has to take the trials for the HIV cure.
Science is informed through a learning curve everyday.
The second process can take place outside the patient’s body, this is known as ex-vivo.
“Gene therapy can be done as ex-vivo, outside the body, genetically modified with no need for a donor. The cells are taken from the patient again, so no challenges of matching donor, no fear of rejection of the cells because they belong to the patient. When modified, the cells are planted back into the bone marrow,” said Dr Kityo who took questions to clarify any misunderstanding.
“Then with in-vivo, an injection is given, this is the goal, we are not yet there, we will get there one day. Currently, we are working on ex-vivo. The two procedures, ex-vivo and in-vivo require no donor.”
Cost
The gene therapy clinical trials have all taken place in the United States and Europe due to the high costs required.
Southern Africa, which suffers the burden of HIV, is not able to finance the procedure.
The tools, the reagents require state-of-the-art equipment making the procedure a dream for Africa currently. However, the expertise is there with Uganda already undertaking the studies.
The US government spent US$2,6 billion on HIV Cure Research in 2020.
In Uganda, starting point is effective tools with plans to have meaningful strategies spelled out in the WHO gene therapy guidelines.
Benefits
With gene therapy pipeline booming, where a donor was required for stem cell transplant, research studies show that no donor will be required for HIV gene therapy, the patient’s genes will be used in the procedure.
While ARVs manage symptoms, suppressing the HIV virus, gene therapy will be a cure.
An injection will be given two months apart with a possibility of two jabs a year with monitoring.
Gene therapy is handy as a possible cure for HIV.
People living with HIV will be able to live without taking drugs because their cells would have been restored. Gene therapy becomes a functional HIV Cure.
Funding
With the Global Fund (GF), calling for ending Aids by 2030, the 2022 to 2025 funding requires US$18 billion. Ending Aids by 2030 implies that HIV treatment will be generalised. Anyone infected will be treated like any patient seeking services for a headache or diarrhoea.
With 1.2 million people living with HIV in Zimbabwe, if funds and facilities permitted, finding willing participants to a cure would not be a challenge.
Personal
As a journalist living openly with HIV, I have a new lease of life. My sincere gratitude to science and all who took part in the clinical trials.
Regimens keep improving, today, a single triple combination pill suppresses the virus. A decade ago, these were three separate tablets.
Viral suppression has led to normality, however, the pill burden remains.
“Someone took the HIV treatment clinical trials for the restoration of my health. I am happy to participate in the cure journey as a participant and journalist,” she said.
HIV cure becomes a reality in my living years.
Currently, less than 15 percent of patients on ART programmes in Africa are on second-line, ritonavir-boosted protease inhibitor (PI) regimens, but this proportion will increase significantly over time.
Recent studies have shown that most patients failing second-line ART in resource-limited settings do not have major PI resistance-associated mutations. (UNAIDS 2020 report).
This means that failure is due to poor adherence rather than the development of resistance.
However, with more patients failing on second-line ART regimens for longer durations this will likely change. The threat of “untreatable” multi-drug resistant HIV after second-line failure in Africa is a cause of concern.
The Ministry of Health and Child Care (MoHCC) stated that as at June 30, 2022, Zimbabwe had 49 944 on second line regimen with 489 on the 3rd line.
The third line being the last treatment, anyone failing that books a berth in the cemetery.
A cure is needed like yesterday, science is at work and this will be a reality one day.








Comments