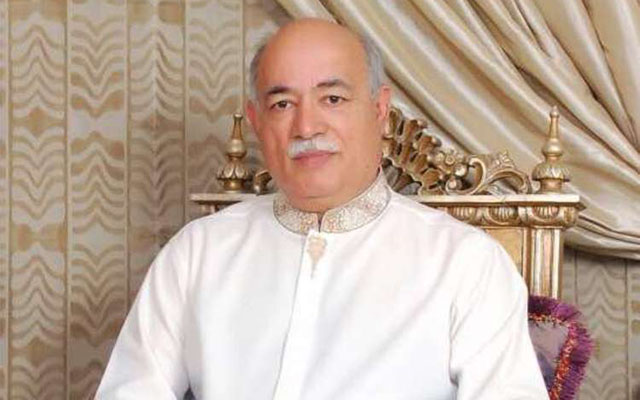
We need paradigm shift in health sector: Shah
Runyararo Muzavazi & Tatenda Charamba Features Writers
Access to health services has become a major issue in Zimbabwe, especially in the advent of non-communicable diseases, which are also known as silent killers. More needs to be done in the health sector for people to be alert and stay healthy. Our features writers Runyararo Muzavazi (RM) and Tatenda Charamba (TC) speak to Dr Bilal Shah (BS), a health expert originally from Pakistan, who has settled in Zimbabwe, on the development of the health sector in Zimbabwe, its challenges and what can be done to improve it.
RM/TC: Why did you come to Zimbabwe and when?
BS: I came to Zimbabwe in 1982 to Parirenyatwa Hospital where I rotated in different specialities. However, I started my practice in July 1987 in the high density areas. Zimbabwe by the time of Independence had a lot of specialists who went outside the country and that is when I was told that a lot of doctors and specialists were needed in the country.
RM/TC: What have you done in the past to improve the health sector in Zimbabwe?
BS: I was the first foreign doctor to work in the high density areas which was dominated by black doctors. I educated people as I went to schools to deliver lectures on good health practices. In 1992, I was introduced to Reuben Barwe (a ZBC reporter) who asked me to deliver a programme on ZBC and I was interviewed on 14 topics. I was then asked to continue the programmes as an anchor and I accepted. I started that programme, “You and Your Health”, in 1992 and it ran up to 2007. I interviewed many doctors and specialists in the health profession and I had the honour to interview Dr Christian Bernard (the South African surgeon who performed the world’s first human heart transplant in 1967).
RM/TC: How did these programmes you carried out on ZBC help the people health wise?
BS: During those days, almost 100 percent of people were watching ZBC, be it in urban areas and some rural areas. As a result of these programmes, we experienced rapid improvements in health and nutrition and improved living standards in the long run which provided the essential basis for improved health. Undoubtedly, much change stemmed from scientific advances, immunisation being a prominent case. Moreover, people prefer traditional health because they say it is affordable compared to medical health.
RM/TC: Where do people go wrong in maintaining their health?
BS: People go wrong when they do not regularly visit the hospital for medical check-ups to see if there are no sprouting diseases in their systems. Also, eating disorders, where people eat unhealthy and do not check their diets. One needs to know their allergies and how to maintain their health. Moreover, people need to know that exercising is not for weight loss, but to keep fit, and I have noticed that out of 10 only three people exercise, which is not good.
RM/TC: Zimbabwe has been faced with drug inadequacies in the last few years, which has impacted negatively on the health delivery system. What has been causing that?
BS: There are no shortages for the basic medicines like antibiotics, but for the anti-retrovirals it’s because they require foreign currency and because of the economic hardships we are facing it has become a bit difficult to insure adequate supply. In addition, the fact that people are not diagnosed at an early stage in the case of cancer has increased the shortages, as they visit the hospitals when their diseases are at an advanced stage, straining the supplies of medications, as well as the increase in second line treatment patients which led to the shortage on anti-retrovirals.
RM/TC: How can the health sector in Zimbabwe be improved, especially to ensure access for all?
BS: Because of the economic hardships being experienced there is need to maintain what we have. Zimbabwe has an advantage of having the best infrastructure on health issues from local health institutions to the satellite clinic and from the special clinic to the hospital. There is need to develop and implement national standards for examination by which doctors, nurses and pharmacists are able to practice and get employment. There is also need to rapidly develop and implement national accreditation of hospitals; those that do not comply would not get paid by insurance companies. However, a performance incentive plan that targets specific treatment parameters would be a useful adjunct. We can also obtain proposals from private insurance companies and the government on ways to provide medical insurance coverage to the population at large and execute the strategy. It is healthy to have competition in healthcare, and provide health insurance to the millions who cannot afford it. Utilisation and application of medical information systems that encourage the use of evidence-based medicine, guidelines and protocols, as well as electronic prescribing in inpatient and outpatient settings. Perverse incentives between specialists, hospitals, imaging and diagnostic centres on the one hand and referring physicians on the other need to be removed and a level of clarity needs to be introduced. Revise the curriculum in medical, nursing, pharmacy and other schools that train healthcare professionals, so that they too are trained in the new paradigm and develop partnerships between the public and private sectors that design newer ways to deliver healthcare. An example of this would include outpatient radiology and diagnostic testing centres. The Government should appoint a commission which makes recommendations for the healthcare system and monitors its performance.
RM/TC: Should we incorporate the conventional health delivery system and the traditional health delivery system?
BS: If that can develop the health delivery sector then why not, because there some diseases that the traditionalists can cure, as well as the modern health care. We can incorporate the two by saying the traditional health specialist can help the people to a point where they can and when it reaches a point where the health condition needs medical attention, they should direct the people to visit the hospital.
RM/TC: A lot of people do not go for early detection of diseases, the general medical check-up. What do you think are the reasons why people shun this noble exercise?
BS: Ignorance due to lack of education contributes significantly to lack of participation by people. Facilities in the country are also insufficient and the ones that are there cannot be afforded by most people. It is always better to have every disease detected early for better management, Non Communicable Diseases cannot be easily picked if no tests are done.
Hypertension is a silent killer and people with the disease may not know it. In some events, the intensity of blood pressure may be very high and if the patient is not taking the medicine, it may result in stroke. In Africa we see more of the stroke, in Indian and other countries like Pakistan we have more of the heart problem. Then the other thing is when the doctor prescribes the medicine and the person feels better, due to some reason, laziness, ignorance and limited resources, the person defaults and stops taking the medicine. When they don’t take the medicine then we have more problems than before.
In any case, HIV has no cure. We are giving the medicine to reduce the virus load. That does not mean the person should stop the medicine after feeling alright. The medicine must be taken regularly. Now, it is so easy because it is one tablet a day so far in Zimbabwe. We have one tablet a day for most of the diseases like diabetes, hypertension. We only give added medication if the patient’s condition is not improving. In the case of HIV, if, in spite of the medicine that the patient is getting from clinics or private sector, if they are still sick we check the virus load and the CD4 count. If the virus load is not decreasing and the CD4 count is not improving then we have the fourth line of treatment to reduce that.
RM/TC: What do you think are the health delivery setbacks in the country?
BS: They are all linked to the economy. Sometimes in the local clinics medicine is not available and at that time a person can go to the nearest pharmacy to get the same medicine, but he or she must take the medicine regularly. In good times people were happy and everything was for free and even Parirenyatwa Hospital offered free services.
RM/TC: What responsibilities should health experts like you shoulder in an effort to ensure the health delivery system is at the desired standards?
BS: Education is very vital and our responsibility as the medical stuff is to deliver lectures on health and expectations to different areas, especially rural areas. In this coming rain season, bilharzia is common, so information on how to protect people from this disease should be spread. There should be provision of safe food and safe water so that people don’t expose themselves to health risks through what they consume.
RM/TC: What are the rules that govern doctors in service delivery?
BS: We should respect the community and be ethical in our operations. There is always a need to check that a doctor is competent enough to diagnose and treat the patient. If they do not have the capacity, there will always be a senior doctor to assist and guide.
RM/TC: We understand you have a programme that is coming soon in your efforts to ensure people have access to health services. Can you elaborate on this?
BS: This programme will help spread information about health to various communities. We will be focusing on preventing and curing of diseases when a risk comes. This will be an opportunity to give answers to health questions so that people of Zimbabwe are protected from diseases. Various media channels will be used and we will also be moving around in different areas where we are able to reach out to people. We will also be visiting schools to assist children with information on diseases and how they can prevent them.









Comments