Obstetric fistula patients suffer below the radar
Francisca Sibanda Chamunokara Correspondent
The word “fistula” is a collective medical term for any abnormal connection between two bodily organs. For almost three years, Sheila Mutengwa (51) was at Harare Central Hospital day after day; month after month with a condition that had puzzled her and her family out of their wits. Urine streamed out of her uncontrollably. The unexplained incontinence, that destined to plague her, resulted in her emitting a foul smell.
By the time Mutengwa was seen by an Ethiopian-based Fistula surgeon Dr. Ambaye Wolde , a specialist from Women and Health Alliance (WAHA) in July this year she could hardly walk because she had not used her legs in such a long time as a result of oozing out water.
She remained seated at her bed all the time.
She eventually developed vitamin B12 deficiency. Surprisingly she was told she didn’t need surgery just medication, vitamin supplements, vaginal muscle exercises and rehabilitation. She is now recuperating in Kadoma old people’s home.
Mutengwa is one of a growing number of women, who suffer from fistula, a little known condition which the World Health Organisation (WHO) describes as “the single most dramatic aftermath of neglected childbirth.”
The word “fistula” is a collective medical term for any abnormal connection between two bodily organs.
In the case of obstetric fistula it is the result of pressure exerted by the foetal head in the pelvis during obstructed labour, a force that interrupts the blood flow to nearby tissues in the mother’s pelvis, resulting in two classifications; Vesicovaginal Fistula (VVF) and Rectovaginal Fistula (RVF).
The two types of obstetric fistula that can occur are: Vesicovaginal Fistula (VVF) occurs when the blood supply to the tissues of the vagina and the bladder is restricted during prolonged obstructed labour, the tissues die between these organs, forming holes through which urine can pass uncontrollably. Rectovaginal Fistula (RVF) occurs in a similar way to VVF, however, holes form between the tissues of the vagina and rectum, leading to uncontrollable leakage of faeces.
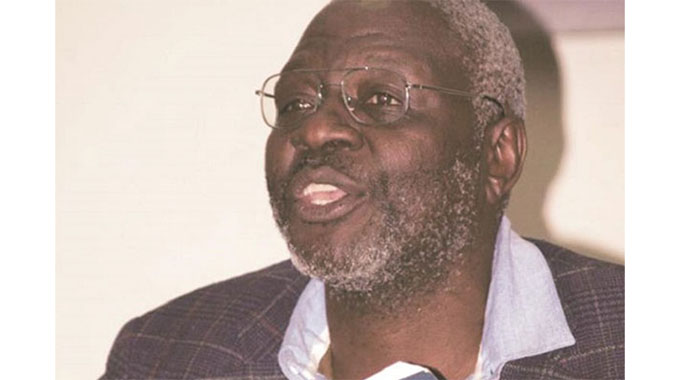
Dr Ladislous Chonzi, a local urologist, says although VVF is not life threatening, it, to a very large extent, affects the quality of life led by an affected woman.
“How can a woman lead a normal life whilst oozing out faecal matter and urine uncontrollably?” he asks.
The government through the Ministry of Health and Child Care needs to place higher priority on this topic. It appears that government itself is not aware of the actual number of sufferers of this disease. Rather authorities seem to push the issue of fistula under the carpet while focusing on other diseases.
According to the World Health Organization (WHO), an estimated two million young women are living with untreated obstetric fistula in Asia and Sub-Saharan Africa. Many of these women live in silence with the treatable medical condition, which can lead to bladder and skin infections, kidney disorders and at times death if left untreated.
According to Chonzi ,VVF affects the lower end of the social strata were expectant mothers either stay too far from a local hospital or they cannot afford private medical care.
“You don’t get such conditions in the private sector” Chonzi said.
In the pre-colonial era VVF was prevalent because of lack of adequate health facilities and telephones were not accessible to remote areas. Women would walk for long distances whilst in labour and to those that had complicated or obstructed labour they wound up with VVF.
In recent years the numbers of cases of VVF are on a significant rise due to the harsh economic times. Many expectant mothers cannot afford delivering in a clinic or hospital. There are several other reasons why expectant mothers may not deliver in a hospital setup but poverty among others is the reason.
“VVF is trauma giving birth,” says Sister Rudo Mutekedza, the only Stumol therapist (wound care manager) in Zimbabwe. As a stomal therapist she is responsible for helping patients adjust to living with either a permanent or temporary stoma (hole) be it a colostomy (a surgicalprocedure where a portion of the large intestine is brought through the abdominal wall to carry stool out of the body.), ileostomy (a surgical opening constructed by bringing the end or loop of small intestine out onto the surface of the skin. Intestinal waste passes out of the ileostomy and is collected in an artificial external pouching system which is adhered to the skin. Ileostomies are usually sited above the groin on the right hand side of the abdomen) or urostomy (Surgical construction of an artificial excretory opening from the urinary tract.)
Her role includes pre-operative counselling, immediate post-operative care and education and follow-up assessment and counselling following patient discharge. As a wound care manager she assesses and implements the management of complex wounds. She has an in-depth knowledge of contemporary wound care practices and healing products.
Mutekedza says VVFs are prevalent in the rural areas or places where women are delivered by a midwife at home. Because some of these midwives are not as thorough as they ought to be, complications quite often occur.
Midwives are supposed to check if the bladder and rectum are empty before the mother starts pushing. They are also supposed to assess the pelvis as to whether or not it can accommodate a baby. A mother can rapture the vagina, bladder or rectum and babies can die in the birth canal and slip out, if the above are not checked.
“For a good number of women who get the disease their husbands abandon them because of the unpleasant odour emanating from the faecal matter and the urine” says Mutekedza. Once abandoned, many of the women face further challenges including the inability to afford sanitary ware to use for their conditions.
The number of the women who came forward from around Zimbabwe for treatment this year in July alone is enough to cause alarm. Mutekedza’s records shows that over 300 girls have come forward in need of assistance in form of VVF repairs. She believes there are more of them out there who may not have access to a health care facility who are very poor as well as those who belong to sects that forbid going to a hospital. The government through the ministry of health needs to address this issue immediately.
Although the new Constitution of Zimbabwe, Amendment No. 20 section 76 clearly states that “every citizen and permanent resident of Zimbabwe has the right to have access to basic health-care services, including reproductive health-care services”; people with fistula are finding difficulties accessing treatment. There is no fistula foundation neither is there much recognition or talk about this traumatic condition.
Mutekedza and her team locate women affected with fistula through social welfare because no one wants anything to do with someone with a foul odour. These women find themselves being ostracized by families and communities. They cannot afford soap to wash as many times as they need to manage the odour.
Those VVF patients who are referred to Parirenyatwa or Harare Central Hospital where repair treatment is supposed to be booked for them, are often repeatedly told to come back. They keep coming back months after months sometimes even for years all in vain.
Andrew Strang a social worker from the UK who is working for the Woman in Health Alliance (WAHA) which is based in Kenya has been working alongside Mutekedza to access hospital records and locate these patients.
Their efforts culminated in the first fistula camp in December 2013 and also another in July this year where, close to 60 women were repaired and attended to. The women gathered at Parirenyatwa Hospital as they were attended to by Dr. Ambaye Wolde Michael of WAHA. The women came from outside of Harare with some coming from as far as the Mozambican border. According to Strand, most of them had been on the waiting list for months.
“When you first met the women they had a very low self-esteem because of the trauma they went through. They were in a deep dark place but after the surgery there was a glimmer of life. The repair gave them hope again”, he explained.
One woman in particular had one of the worst cases and she was also the youngest of the group. *Regina who is now 19 say when she was 16 she was impregnated by an elderly married man in their neighbourhood. When she was eight months pregnant the wife found out and came to assault her which sent her into premature labour. She was delivered by her grandmother at home. The labour was long and hard. Eventually the baby slipped out, dead leaving her with a raptured bladder and rectum. For three long years she oozed out urine and faeces uncontrollably.
“Nyangwe ndisina kunwa mvura chero tea mvura yacho yaingojuja (even without drinking any water or tea, urine just continued to gush out)” she narrated.
After the repair she sits looking out the window. Her eyes are filled with life and hope. She’s lively and bubbly again just like any normal teenager.
There was another fistula camp last week from December 8 to 12. Dr Ambaye came again to do more repairs on about 20 women. WAHA plans on holding week long fistula camps every 3 months in the following year. This is necessitated by the number of women who are reaching out in need of repairs.






Comments